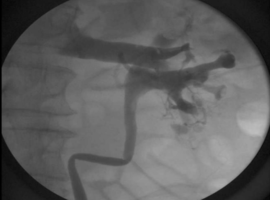
An 84-year-old male with past medical history of Ta Low-grade urothelial cell carcinoma (UCC) diagnosed in 2020 via TURBT without recurrence, BPH, and aortic stenosis s/p aortic valve replacement presented secondary to new onset gross hematuria plus severe left sided flank pain. Examination showed a male in no acute distress with a benign abdominal exam. Creatinine was 2.7, increased from a baseline of 1.7. Hemoglobin was 12.4 which was consistent with the patient’s baseline. Vitals signs were within normal limits. CT of the abdomen and pelvis without contrast showed multiple areas of hyperechogenicity within the left collecting system accompanied with mild left hydroureteronephrosis. The patient then underwent cystoscopy and left retrograde pyelogram (Figure 1). Given intraoperative findings, a left ureteral stent was placed with a foley catheter. Several days later, diagnostic ureteroscopy was performed. No fistula was identified, but rather, an upper pole papillary lesion measuring 2cm. Endoscopic biopsy was performed revealing papillary renal cell carcinoma (RCC), Furhman grade 2. The patient did ultimately undergo robotic assisted laparoscopic left radical nephrectomy with final pathology showing a 2cm papillary mass extending into the collecting system, consistent with pT3a papillary RCC, Furhman grade 3.
Discussion: This is an unusual occurrence of a suspected venocalyceal fistula. Exact etiology is often unknown, but venocalyceal fistulas have been reported to occur after renal transplantation and percutaneous nephrolithotomy, or from chronic ureteral obstruction [1-3]. We hypothesize that the obstruction from the lesion increased intra-calyceal pressure greatly enough to induce a small fistulous connection. Given the degree of contrast passage into the renal vein, we suspect there was a small venocalyceal fistula that resolved with ureteral stenting and collecting system decompression. The management of venocalyceal fistulas can often be conservative and requires treatment of the underlying issue, such as in this rare scenario.
Conclusion: This is an exceptionally rare retrograde pyelogram finding of a venocalyceal fistula in the setting of malignant obstruction. The case details a fascinating imaging finding and correlative management which can assist future decision-making for clinicians in similar, and perhaps unexpected, scenarios.