Deep morphea is a form of localized scleroderma in which inflammation and sclerosis are found in the deep dermis, panniculus, fascia, or superficial muscle, typically in the face, trunk and limbs [1]. Associated clinical findings, including arthralgias, arthritis, contractures, or carpal tunnel syndrome, are frequent and rarely visceral manifestations may occur [1]. Eosinophilia, hypergammaglobulinemia, increased erythrocyte sedimentation; rheumatoid factor, antinuclear antibodies (ANAs) and anti-dsDNA, anti-histones, anti-nucleosome, anticardiolipin antibodies have been reported. Etiology is still uncertain and treatment options are unsatisfactory but include NSAIDs, antimalarial agents, topical and systemic corticosteroids, PUVA, vitamin E, vitamin D3, aminobenzoate potassium, penicillin, retinoids, interferon-gamma, D-penicillamine, methotrexate, cyclosporine, mycophenolate mofetil, cyclophosphamide, azathioprine, bosentan, IV immunoglobulins, abatacept, tocilizumab and rituximab [1,2].
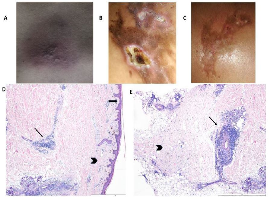
A 42-year old woman went to the rheumatology outpatient clinic, complaining of inflammatory polyarthralgias and lumbar pain, without Raynaud phenomenon history or other systemic symptoms. Physical examination revealed polyarthritis and a hyperpigmented, mildly inflamed and thickened skin in the lower lumbar region (Figure A). She had no sclerodactyly, nor telangiectasias. She presented with raised inflammatory markers; normal blood count, renal and hepatic functions. Its seronegative polyarthritis remitted under methotrexate 20 mg/week, prednisolone 10 mg/day and etoricoxib 90 mg/day. However, the localized skin thickness worsened during several months. Nailfold capillaroscopy remained unremarkable and she evolved with positive direct coombs test, lupus anticoagulant, ANAs (1/320; homogeneous), anti-dsDNA (130,1 U/mL), anti-nucleosome and low titre anti-beta-2-glycoprotein I and anticardiolipin antibodies. The diagnosis of deep morphea was based on the clinical and histopathological findings (Figure D and E) and she began on hydroxychloroquine. Unfortunately, skin biopsy complicated with ulcerations (Figure B) with impaired healing that is slowly improving (Figure C).
Therefore, this is an interesting clinical case of a rare type of localized scleroderma, with an atypical localization and refractoriness to some of the first-line treatments, which became a challenge for the clinicians.